Should I Get a Root Canal Treatment or a Dental Implant?
What is the Difference Between a Root Canal Treatment and a Dental Implant?
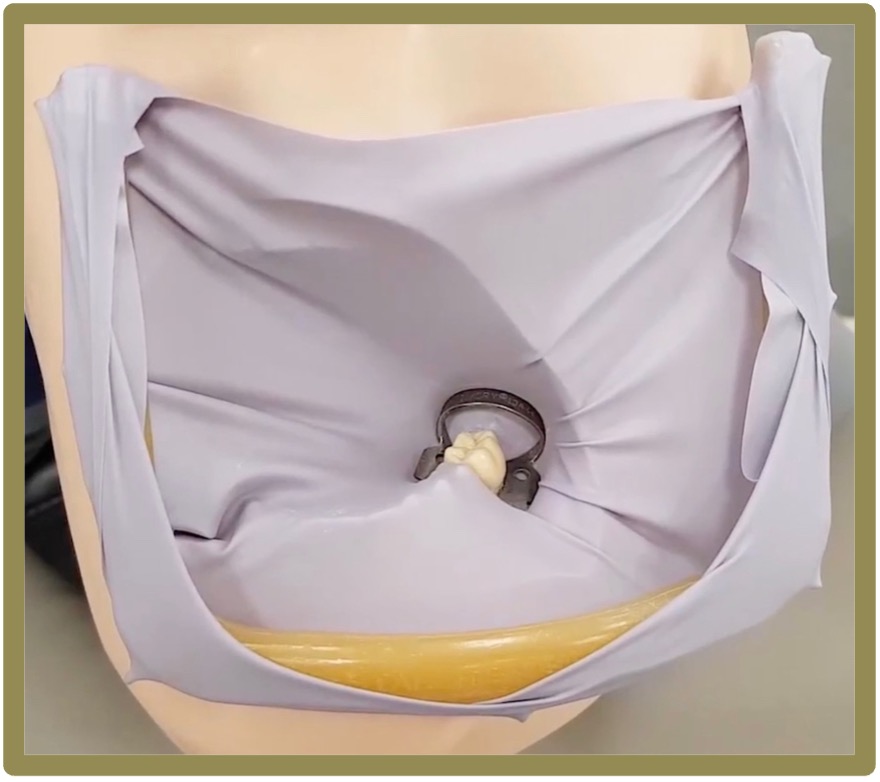
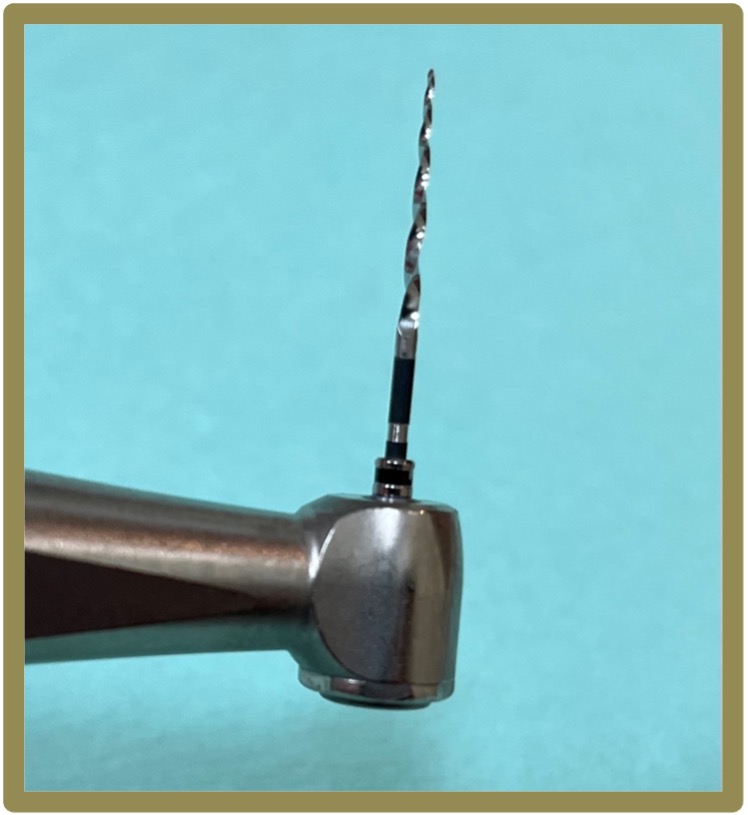
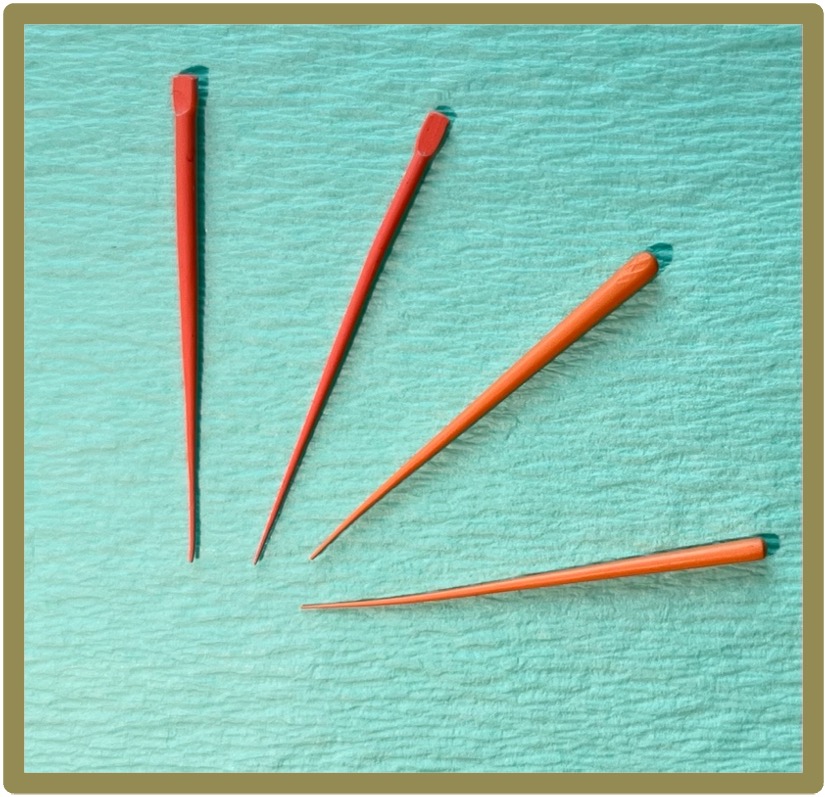
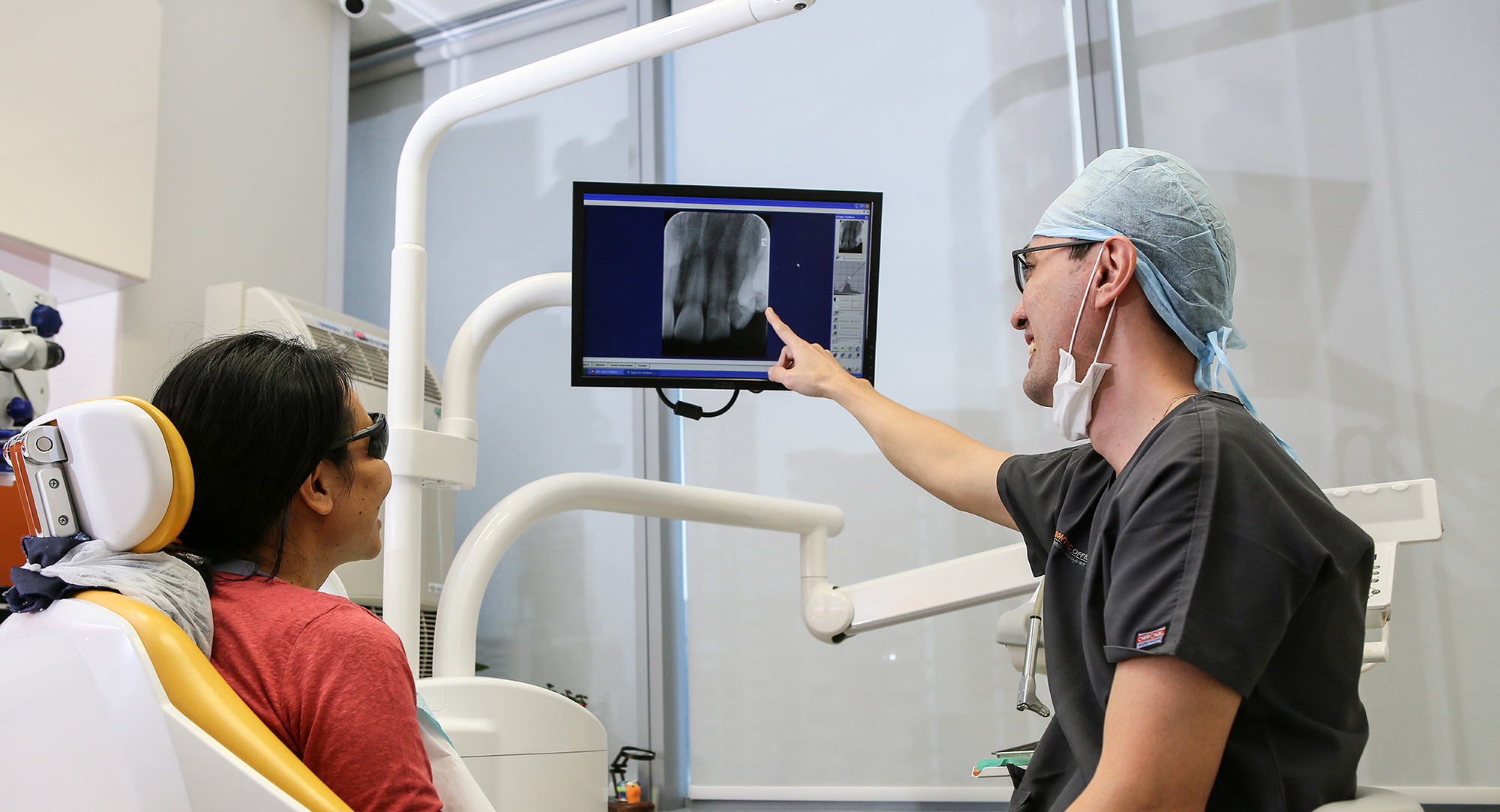
Root canal treatment, also known as endodontic therapy, is a procedure performed to save a tooth that has an inflamed or infected pulp – the tooth pulp consists of the nerves and blood vessels in the innermost part of the tooth. The procedure involves removing the diseased pulp, cleaning and disinfecting the root canals, and then sealing them with dental materials to prevent further infection. This procedure is typically recommended when a tooth can be preserved and the surrounding bone is healthy enough to support it. Hence, root canal treatment is aimed at preserving the natural tooth, addressing the issue of infection while keeping the natural tooth structure. For more information, feel free to browse our blog posts: “Root Canal Treatment Procedure: What Should You Expect?” and “I Am Having a Toothache – What Should I Do?”.
Dental implant treatment, on the other hand, is a restorative option for replacing a missing tooth. For the implant to be placed, the diseased tooth has to be removed. The dental implant procedure involves the surgical placement of a titanium implant into the jawbone, which serves as an artificial tooth root. After a period of osseointegration, during which the implant fuses with the surrounding bone, an artificial crown is placed on top to simulate a natural tooth.

A radiograph illustrating an implant prosthesis that replaced an upper front tooth.
How Does the Longevity of a Root Canal Treated Tooth Compare with a Dental Implant?
A successful root canal treatment can extend the life of a natural tooth for many years, even decades, if proper oral hygiene is maintained and the tooth is adequately protected with a crown where it is deemed necessary.
Long-term studies have shown that root canal-treated teeth and dental implants have comparable longevity, with dental implants potentially needing more maintenance procedures than root canal-treated natural teeth. It is important to note that dental implants are not immune to developing gum disease around them, which might lead to progressive inflammation or infection of the gums and bone around the implant and may result in the eventual failure of the implant. Studies have shown that smokers, who are at higher risk of developing gum disease, are more likely to suffer a dental implant failure than to lose a natural tooth to gum disease.
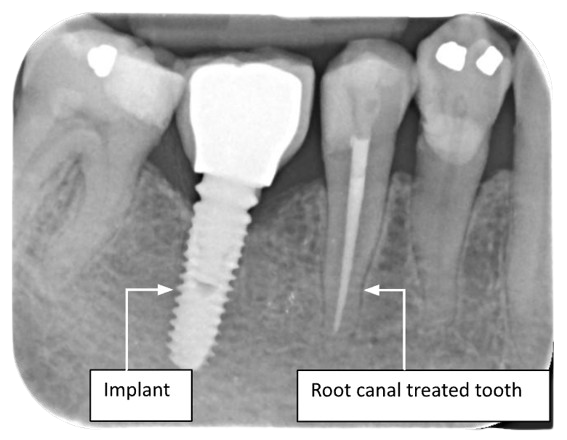
A radiograph illustrating an implant prosthesis and a root canal treated tooth.
Am I Suitable For Root Canal Treatment Or Dental Implant Treatment?
Both procedures require careful consideration of the patient’s overall oral health and specific circumstances. Root canal treatment is generally more conservative, as it aims to preserve the natural tooth, and should always be considered as a first-line treatment approach to managing a diseased tooth whenever possible. However, should the diseased tooth be severely compromised, such as having very deep cracks or fractures that make the tooth unsalvageable, then extraction of the tooth needs to be carried out, and a dental implant may be considered as a tooth replacement option following the loss of the tooth.
Dental implant treatment requires adequate jaw bone thickness and density for proper integration and may not be suitable for everyone or every jaw site. In addition, there are some medical conditions that may make a patient unsuitable to receive dental implants, such as osteoporosis, as well as the use of antiresorptive medications, a history of radiation therapy to the head and neck, and uncontrolled diabetes.
Conclusion
In conclusion, root canal treatment and dental implant treatment are two distinct procedures with different objectives. Root canal treatment aims to preserve the natural tooth by treating the diseased pulp, while a dental implant is an artificial tooth that is installed in the jaw bone after a diseased tooth is extracted. Both procedures, when performed by skilled professionals and maintained well with good oral hygiene practices, can be equally successful.
Generally, root canal treatment may be considered as a first-line treatment for a diseased tooth, whereas tooth extraction followed by a dental implant should be viewed as an alternative or last resort for individuals with a tooth that is severely compromised or unsalvageable. It is important to note that not all patients or jaw sites may be suitable for dental implants. Additionally, if a dental implant should fail subsequently, the patient will often need to consider other prostheses, such as a dental bridge or a removable denture, since a repeat implant procedure at a previously failed site is unpredictable.