- Home
- /
- FAQ
What is the tooth pulp and how it is related to toothache?
Toothache is usually a term that is used to describe pain from the tooth and it can be a disease involving the tooth pulp or the pulp space.
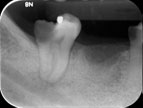
Decay near to the pulp and can potentially cause toothache.
Pulpitis can exist in several forms. Sometimes mild pulpitis can persist as very sensitive tooth and can gradually subside over time. In severe pulpitis, the pulp may not be able to heal and the bacterial infection will overwhelm the vitality of the tissue. The infected tissue within the root canal space will soon cause inflammation or even infection of the bone and gum tissue around the tooth root. That is the reason why long progressing toothache can cause pain and swelling around the gums of the tooth.
When is root canal treatment required?
Root canal treatment is indicated when pulpitis or infected tissue have been diagnosed. In most instances, the diagnosis can be arrived with proper examination.
There are situations whereby the pulps are neither inflamed nor infected but are electively removed to prevent occurrence of toothache or swelling.
Is root canal treatment procedure painful?
Local anaesthetic has to be given before the start of the procedure. Otherwise, root canal treatment can be painful. There are several techniques that are used to numb the tooth before root canal treatment proceeds. In some cases, the infection or the pre-existing pain may cause the tooth to be more resistant to anaesthetic, hence the clinician may need to adopt more measures to provide adequate anaesthesia.
In our clinic, we have adopted techniques and supplemented with state-of the-art machines to deliver less painful injections.
What do I expect after root canal treatment?
Transient pain can occur following root canal treatment and can be adequately controlled by oral painkillers.
Uncommonly, there can be swelling from the tooth following root canal treatment. This is especially so when there pre-existing infection of the tooth. In such situations, the clinician will probably need to supplement the painkillers with antibiotics.
Does root canal treated teeth need special care?
Root canal treated teeth have a higher tendency to fracture. Patients are routinely advised not to bite hard foods with the treated tooth before a crown or a final restoration is placed.
The outer hard structures of the root canal treated teeth still remains as they originally are and they can still be affected by tooth decay or gum disease. Routine oral hygiene habits like brushing and flossing should still be continued.
Are radiographs necessary and will it impact on my health?
In the course of a root canal treatment, several radiographs are taken to achieve good standard of care. This is to ensure each step is properly checked so that the best possible outcome can be achieved. The radiation dosage is low and one exposure of digital peri-apical radiograph is probably comparable to several hours of background radiation under the sun. Dental surgeons with good knowledge in oral radiology would advise that radiation in dental x-rays should not be detrimental to good health.
My tooth was root canal treated tooth and my dentist advised me to retreat it. Why is that so?
Root canal treatment usually has good success rates. Nevertheless, success rate depends on the pre-existing condition of tooth.
When root canal treatment fails, it usually presents persistent inflammation of the bone and may sometimes give rise to swelling and pus discharge. Below are some of the reasons why root canal treatment fails:
- Persistent or recurrent root canal infection. This may occur even after a good root canal treatment has been performed. The assessment of re-treatment will be based on the quality of root canal filling, the status of the disease and the nature of the signs and symptoms.
- Defective fillings that may compromise the sealing ability of root canal fillings from bacteria.
Redoing root canal treatment is usually more challenging. This is due to the presence of materials that are usually difficult to remove.
What are the success rates of root canal treatment?
Root canal treatment does not confer 100% success rate, like all other medical procedures. However they are generally good and arguably better than that of implants in certain instances. The success rates of each individual case varies and can be judged based on the pre-existing condition of the tooth.
There are 3 categories where success rate can be judged:
- Teeth with no prior infection : success rate can be over 90%
- Teeth with pre-existing infection but had no previous root canal treatment done: There are many studies and success rate varies. It can be communicated to patient that success rate of such teeth is around 80%
- Teeth with previous root canal treatment done and there are signs or symptoms of infection: success rate are much lower than the previous group.
Redoing root canal treatment is usually more challenging. This is due to the presence of materials that are usually difficult to remove.
How do I know when root canal treatment fails?
The obvious situation would be persistent or re-emergence of signs and symptoms.
The best way to tell if a root canal treatment is successful is to take a radiograph to see if the inflammation previously caused by the infection of the root canals is subsiding or has subsided. If there was no previous inflammation, then the intention of radiograph examination is to check if there is emergence of inflammation.
Usually the radiographs are taken 6 months after completion of root canal treatment. The reason for that is that any signs of inflammation subsiding or emerging on the radiograph would be more evident after 6 months.
